
Radius fracture & distal radius fracture
Radius fracture & distal radius fracture Causes, types, and treatment of a broken forearm
An awkward fall is often enough to cause a radius fracture. It’s a knee-jerk reaction to break a fall with your hands. That’s how most of the impact is on the hands and forearms, which can result in the radius fracturing. If pain and restricted movement occur in the hand and/or arm after a fall, a quick diagnosis is important. A radius fracture can have serious complications and should therefore be treated by a physician as soon as possible.
Causes: this is how a radius fracture occurs
A radius fracture can be caused by severe compression, excess pressure applied laterally, a blow to the forearm, or a violent distortion of the forearm. Falling onto the hand or forearm is by far the most common cause of a radius fracture. But traffic or work accidents, too, where the hand and forearm get trapped can result in this kind of fracture.
Those suffering from osteoporosis are particularly vulnerable because the reduced bone density decreases the fracture strength of the bones.
Anatomy of the forearm
The radius is a slender bone covered in rough periosteum. At the top and bottom, the areas supporting the articular surfaces are thicker. These articular surfaces connect the radius in the wrist to the carpal bone, and in the elbow area to the humerus. The ends of the forearm bones also feature articular connections between the ulna and radius that are held together by strong ligaments.
What is a distal radius fracture?

In most radius fractures, it’s the long shaft of the radius that breaks, while the articular connections are not affected. If the radius fractures slightly above the wrist (a maximum of 3 cm away from the wrist), the term is distal radius fracture (distal = away from the body).
We distinguish two types of distal radius fracture:
Typically, a radius fracture is associated with pain, swelling, and restriction of movement. Both fractures can usually be treated conservatively (without surgery).
Radius fracture surgery: when is it needed?
However, radius fractures that affect the ends of the bone forming the joint are usually very complicated. If the wrist is fractured, the joint has to be restored surgically – ideally without the formation of steps in the articular surface – to prevent subsequent damage. Open fractures where the end of a bone pierces the muscles and skin are particularly dangerous. Quick surgery is crucial here for complete recovery.
Diagnosing and treating a radius fracture
The definitive diagnosis of a radius fracture can only be made using X-rays. X-ray imaging will show the physician the position of the fracture and the course of the fracture line. The physician can then recognize, or exclude, the possible involvement of joints. Using X-ray imaging, the physician can also determine whether there are two or several fractured components (fragments), and whether the fractured ends are close together or if there is a large gap between them.
All this information is crucial for the next treatment steps of the injury. If the fractured ends lie cleanly on top of each other – this may be the case when the surrounding periosteum has remained intact – a plaster cast or a splint will be applied and physiotherapy started as soon as possible. If the fractured ends are far apart or have shifted past each other, contact between the fractured surfaces has to be restored using repositioning. If this is achieved without surgery, conservative, early functional treatment can also be started. This initially involves several weeks of immobilization (plaster cast or splint) followed by physiotherapy.
If the fractured ends have shifted a lot or the joint is involved, surgical repositioning is carried out. During this procedure, the ends of the bones are usually connected using metal plates (plate osteosynthesis). Wires are not used as frequently. Plate osteosynthesis has the advantage that the fractured ends are secured soundly straight away, meaning there is no need for a plaster cast. This also means that physiotherapy can begin earlier.
How does an orthosis help heal a radius fracture?
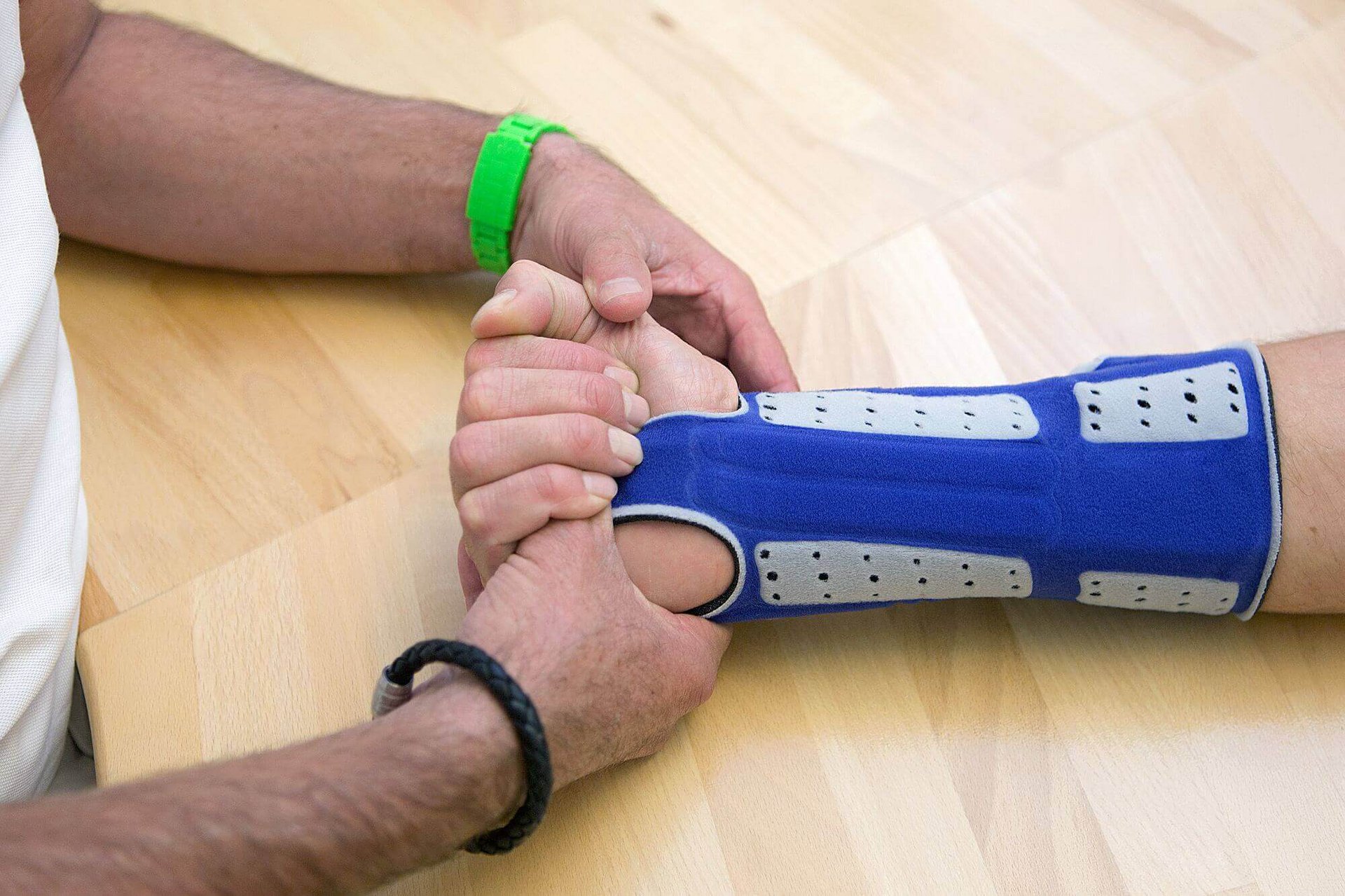
So that those affected can regain their mobility, coordination, and strength as quickly as possible after a radius fracture, and don’t lose those capabilities to begin with, the immobilization phase should be as short as possible. To further treat stable forms of radius fractures – i.e. no ligaments are injured – a wrist orthosis can perform the supporting function of a plaster cast or splint.
The ManuLoc long reliably encloses the injured section of the forearm and thus prevents unwanted movements as well as adverse forces applied on the fracture. While the injured area is being reliably stabilized, the fingers remain mobile, allowing an early start to therapeutic exercises for the fingers and hand.
A wrist orthosis, such as the ManuLoc long, can also ensure additional stability and support after the plaster cast or splint has been removed. This particularly lightweight orthosis secures the wrist in a comfortable neutral position and makes post-operative wound checks as well as physiotherapy easier in order to achieve an overall ideal treatment result.
ManuLoc® long
Stabilizing wrist orthosis with longer lever
Whether carpal tunnel syndrome, acute injuries, post-operative irritation or chronic osteoarthritis: the extra-long ManuLoc long by Bauerfeind immobilizes the wrist but not the fingers and thumb.
To product page