
Varicose veins
When vascular diseases become visible
When superficial veins expand because of blood congestion, and are then visible, mainly on the calves or the inside of the thigh, the condition is referred to as varicose veins. Around one in five adults suffers from this noticeable change in the veins. If left untreated, varicose veins can get worse and result in open ulcers on the leg or, in rare cases, even life-threatening pulmonary embolisms. It’s therefore important to know how to recognize varicose veins, why some forms of varicose veins are dangerous, and what you can do to combat them.
How to recognize varicose veins?
Owing to their characteristic appearance, varicose veins are easily identified: the classic condition of varicose veins (medically also known as “varicosis”) has knotty tortuosities or a cluster of veins that stand out, on the legs in particular, with their blue or purple color. “Spider veins” are a less pronounced form of varicose veins. They are characterized by fine, reddish or blueish “branches” underneath the skin and are therefore mildly reminiscent of spiders. Spider veins, too, frequently occur on the legs and sometimes in the face, but are seen as harmless.
Symptoms of varicose veins
In addition to the visual changes described above, varicose veins can also manifest with the following symptoms:
What are the causes of varicose veins?
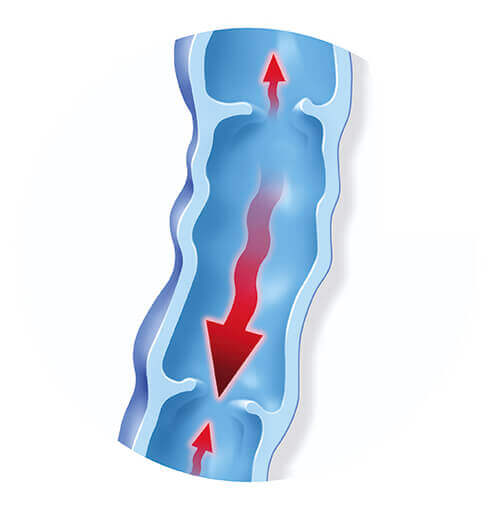
Venous valves ensure that blood is transported exclusively toward the heart. Different factors can be responsible for these valves no longer being able to close properly. Blood then pools in the veins and accumulates there. As a result, pressure on the vein walls increases until they eventually expand, causing the superficial veins to become visible under the skin as varicose veins.
On the one hand, a congenital predisposition to weak veins seems to play a part in the development of varicose veins because they frequently run in families. In this case, the problem is a congenital connective tissue weakness which manifests as spider veins to begin with, mostly from middle age onwards. Physicians refer to this condition as primary varicosis.
If varicose veins do not develop as part of a congenital predisposition but because of an illness, e.g. a deep leg vein congesting as a result of a blood clot (deep vein thrombosis), this condition is referred to as secondary varicosis. On the other hand, a weak heart can also be a cause of varicose veins because blood pools in the veins as the result of an impaired heart beat (right ventricular failure).
These pathological expansions can occur in different areas of the superficial vein system. Physicians therefore use different terms: spider veins, reticular varicose veins, lateral branch varices, trunk varicosis, and varicose veins of the perforan veins.
In addition to genetic factors and pre-existing conditions, the following risk factors can advance the development of varicose veins:

How can varicose veins be prevented?
A healthy lifestyle can reduce the risk of varicose veins: in addition to a balanced diet and sufficient liquids every day, you should also ensure you exercise regularly. Going for a walk, hiking, cycling, swimming, or gymnastic exercises not only help combat obesity but also activate the muscle vein pump.
At work, standing or sitting for extended periods should be avoided as much as possible. We recommend taking regular short breaks for activities, doing foot exercises, or even putting your legs up every now and then to help your leg veins with the venous return of blood to the heart. We also recommend loose clothing, comfortable, flat footwear, and medical compression stockings.
In summer, the vessels expand to help the body cool down. This, however, increases the reflux in veins that are already weakened. To support your veins, you can regularly shower your legs with cold water, resulting in the veins constricting and the blood flowing more quickly.

What makes varicose veins so dangerous?
The progression is different for every patient. If varicose veins remain untreated for a long time, the condition can worsen because the reflux of blood in the veins is a huge strain on the vessel, which continues to increase. At an advanced stage, venous insufficiency can develop which can result in ulcers on the lower legs (ulcus cruris, venous leg ulcers).
There is also an increased risk of blood clots developing in the expanded vein. Such a clot (thrombus) can become fully or partly detached from the vein wall and may then be transported with the blood through the heart and into the fine lung vessels. This causes a life-threatening vascular occlusion, also known as pulmonary embolism. That’s why varicose veins should not be ignored but be diagnosed and treated early by a physician. The risk of severe complications can be significantly reduced in most cases with relevant treatment.
Varicose veins should always be examined straight away by a physician (family physician, phlebologist, or dermatologist) to find possible causes and to prevent the development of dangerous consequential
How are varicose veins diagnosed?
If varicose veins are suspected, a thorough examination by a physician is crucial. The physician will determine whether the condition is a primary or secondary varicosis. The physician must also find out whether deep leg veins are affected or whether the patient is suffering from another condition – e.g. kidney or heart problems – which can also cause water to accumulate in the legs. Various imaging technologies, such as ultrasound, can give an indication of deeper changes.
Treating varicose veins: how can symptoms be combated?
Once the diagnosis is definitive, the physician’s treatment recommendations should be complied with and implemented. These often include:
Furthermore, depending on the condition’s progress and triggers, but also on the patient’s subjective level of suffering and wishes, in consultation with the treating physician, various invasive surgical treatment options are available, such as:
How do medical compression stockings help to combat varicose veins?

Medical compression stockings are used to treat varicose veins, in particular to prevent the condition from worsening and to support the affected veins. They are also an indispensable component of treatment in follow-up care after venous surgery.
In addition, medical compression stockings are incredibly valuable in situations that subject the veins to strain, thus preventing varicose veins and leg vein thrombosis. When external pressure is exerted on the vein, the vein wall can withstand the internal pressure more effectively and the venous valves are able to close again, which prevents further pooling. Compression stockings also boost the return of blood to the heart, thus reducing the risk of thrombosis.
High-quality medical compression stockings, such as the VenoTrain micro or the VenoTrain soft, evenly distribute pressure across the entire surface of the leg and therefore,in addition to the skin-friendly material, provide a high degree of wearing comfort. The stockings are available in standard sizes or as custom-made solutions, as knee-high or thigh-high stockings, and as pantyhose. They are also available in many attractive colors adapted to current fashion trends. This makes them easy to combine with everyday clothing so that they can’t readily be recognized as compression stockings, even at a closer look.
For your compression therapy:
VenoTrain® micro
The versatile compression stocking for a customized style
The VenoTrain micro’s elastic knitted fabric promotes circulation and prevents spider veins as well as varicose veins, even during pregnancy.
To product page
All information provided in this brochure/online (text, images, graphics, etc.) are purely complementary to any advice given by medical experts, in particular the treating physicians or physical therapist. This brochure is not designed to replace this medical advice. We highly recommend obtaining medical advice and following instructions/treatment specified by a physician before using Bauerfeind products or accepting therapy recommendations. Our explanations are not designed to support or promote self-diagnosis or self-medication but are merely there to provide initial general information. Only then can the best possible effectiveness of our products be guaranteed, allowing you to recover quickly.